The first time I heard about Hidradenitis Suppurativa (HS), it was through a friend who had been recently diagnosed. She showed me tracks of ulcers that had developed in her armpit, and admittedly, I recoiled.
Is it contagious? I wondered. Should I ask? I angled my chair just slightly so I could scoot back without making it obvious.
“It’s not contagious,” she said, rolling her eyes. She saw right through me – and I’d never felt so ashamed. “Okay, so what IS it?” I asked, deciding the most direct route was probably the best. We ended up chatting about the condition, how she was misdiagnosed by her family doctor, and how she was now working with a dermatologist to come up with a treatment plan.
Over the next several years, I watched as she went through ups and downs with HS, and how living with the condition affected her mental health, relationships and social life. Eventually, she opted for surgery to expose “tunnels” under the skin. She was the first and only person I’d known who was diagnosed with this condition, but I’ve since learned that HS impacts an estimated 1 million Canadians – possibly more, but many are not accurately diagnosed.
Years later, in 2018, I joined a Twitter Chat that was focused on spreading awareness of HS.
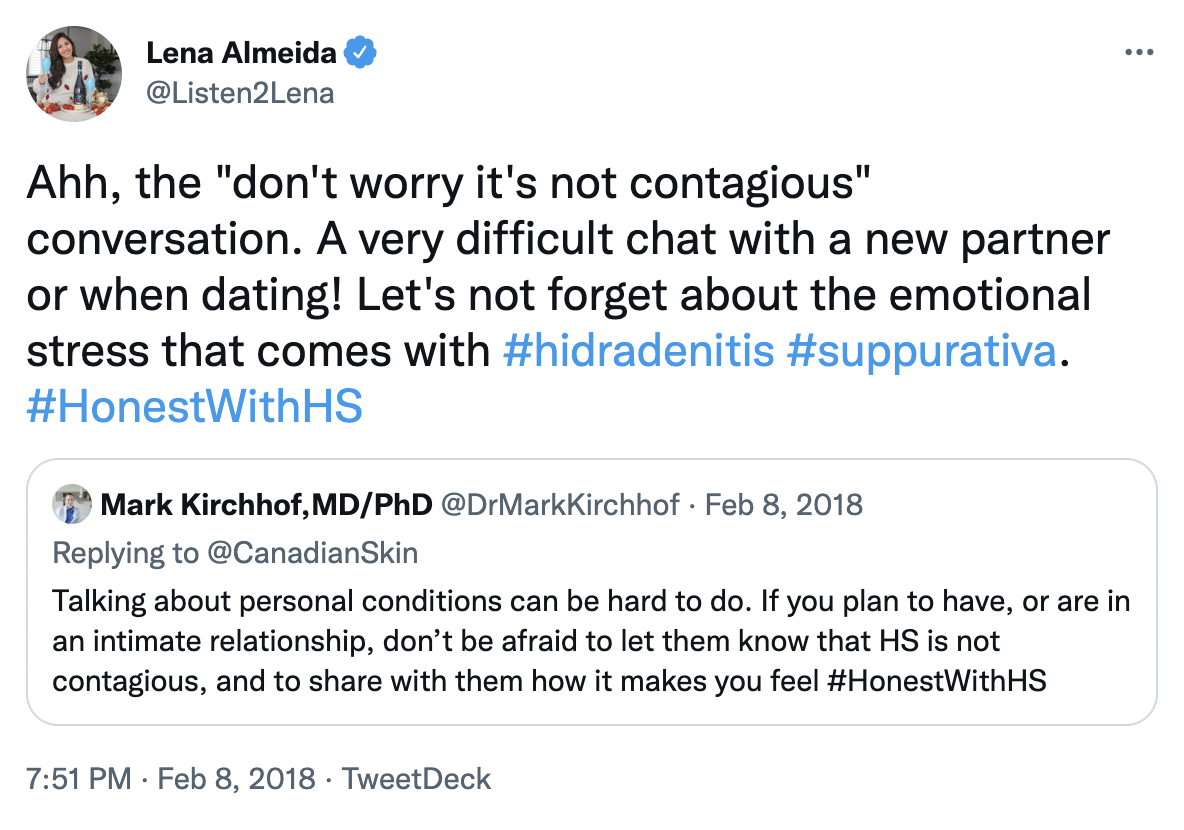 Although I had not experienced the condition personally, I felt that I needed to use my platform to advocate for my friend and help destigmatize HS. It was a successful chat; #HonestWithHS trended in Canada and fulfilled its goal of informing a larger audience.
Although I had not experienced the condition personally, I felt that I needed to use my platform to advocate for my friend and help destigmatize HS. It was a successful chat; #HonestWithHS trended in Canada and fulfilled its goal of informing a larger audience.
It’s HS Awareness Week, and I wanted to once again take the opportunity to talk about Hidradenitis Suppurativa, including a quick Q&A with Dr. Geeta Yadav, a dermatologist based in Toronto at Facet Dermatology.
First, the facts:
– It can take an estimated seven years to be properly diagnosed.
– Due to the symptoms and areas of the body impacted, HS is commonly misdiagnosed as an STI, boil, or other skin infection.
– The condition can be painful, embarrassing and take both a physical and emotional toll on the person impacted.
– There is currently no cure for HS, but the goal of treatment is to achieve good control by reducing the frequency and severity of flare ups so the disease would have minimal impact on quality of life.
I highlighted the first point because it’s the reason this blog post exists: if you suspect you may have HS (see a symptom checklist here), proper diagnosis is key. In fact, you may have landed on this post while searching for more information online. Speak to your healthcare professional and learn when and how to obtain a referral to a dermatologist. Skin doctors are best suited to developing the right treatment plan for your condition.
Next, my Q&A with Dr. Yadav:
What treatment options are available for HS?
Typically, I think of options as topical, oral, injectable and surgical. To reduce flares, patients need to maintain with injectable and topical treatment. Surgery is adjuvant therapy for when areas flare and are difficult to manage medically.
How does the severity of HS affect treatment options?
The more severe the disease (and that can mean because of location or how significant the flares are), the more likely I am to put someone on systemic therapy to help reduce those flares and stabilize the disease. We have only one approved systemic therapy for HS available on the market but I know more are coming down the pipeline. These therapies have changed people’s lives and their ability to function without severe flares.
What are some self-care practices that can have a positive effect on HS symptoms?
Weight loss and quitting smoking are key to improving HS. Obesity and smoking have been directly linked to severity of disease. Friction can also play a role so loose clothing can be more comfortable and reduce the risk of flares. Laser hair removal has shown to be effective depending on the area. Sweating can also be a trigger so treatments for hyperhidrosis can be helpful to manage the disease.
Looking for more information? Resources include:
Canadian Skin Patient Alliance
Canadian Dermatology Association
HS Heroes
Now more than ever, greater awareness and understanding of HS impact and the need for community support are vital. It’s been eight years since I first heard about HS, and after I began speaking about it more openly on my platform, I’ve met many others online who struggle with the condition. Remember, effective treatment options are available, and you are your best advocate. Talk to your health care provider and ask to see a dermatologist.
Leave a Reply